Abstract
Background: The paradigm of the treatment mantle cell lymphoma (MCL) has changed due to development of newer agents (such as ibrutinib, lenalidomide, temsirolimus). Considering that the scheme of using the newer drugs implies permanent drug intake (before disease progression), which helps prevent the early relapses. With a high degree of probability, it can be assumed that MCL, in the future can be withdrawn from the group of aggressive and relapsing lymphomas. Evaluation and monitoring of the minimal residual disease (MRD) in patients with MCL allows to predict the course of the disease and optimize the strategy for maintaining this category of patients.
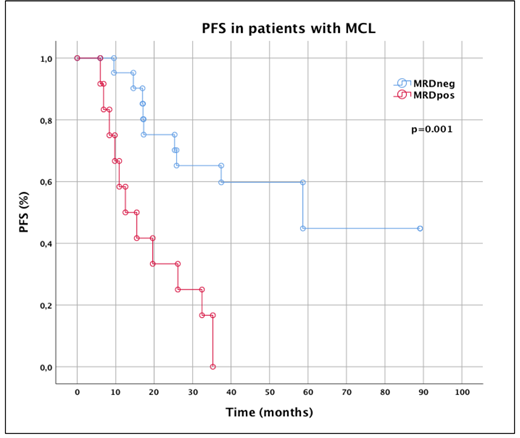
Aim: To assess influence of MRD negative (MRDneg) status on the duration of progression free survival (PFS) and overall survival (OS).
Method: In this study were included 33 patients with MCL (male/female ratio 3:1), age 51 to 82 years (median 64 years). The median of follow-up duration is 80.7 months (range 0.7-147.1). Median of therapy lines - 1 (range 1-5). With rituximab-containing chemotherapy regimens were treated 25 patients (R-CHOP - 12, RFC - 5, RBV - 3, RB - 2, R-DHAP - 1, R-Hyper-CVAD - 1, RVc-CAP - 1); ibrutinib - 3, lenalidomide - 3 and temsirolimus - 1. Autologous stem cell transplantation (AutoSCT) was performed in 7 patients (21.2%). Maintenance therapy received 23 patients (69.7%): rituximab - 20, ibrutinib - 1, lenalidomide - 1 and temsirolimus - 1. During the follow-up period, 9 patients (27.2%) died: progression of the disease - 5, other reasons - 4. The evaluation of MRD status was carried out using 5-color flow cytometry on bone marrow samples after completion of induction therapy. The absent of MRD was detected when less than 1 tumor cell was detected per 10000 leukocytes (10-4).
Results: Complete remission (CR) was achieved in 54.5% (n=18), partial remission (PR) - 45.5% (n=15). Patients were divided into two groups depending on MRD status: group MRD positive (MRDpos) (n=12) and group MRD negative (MRDneg) (n=21). The frequency of achievement of MRDneg status was 63.6% (CR - n=15, PR - n=6). Noted, that all patients (n=7) who underwent AutoSCT achieved MRDneg status after induction therapy and kept it after consolidation with AutoSCT. Disease progression in MRDpos group was state in 11 patients (91.7%), in MRDneg group - 6 (28.6%) (р=0.0005). Patients with MRDpos status who underwent maintenance therapy achieved MRDneg status in 8/12 cases. One patient, after completion R-CHOP + AutoSCT followed by a two-year maintenance program of rituximab, retained MRDneg status. A year later, during the control survey, MRDpos status was recorded. This patient was resumed maintenance therapy with rituximab. MRDneg status is achieved after 6 months from the beginning of maintenance therapy. Median PFS in group MRDneg was not achieved, in group MRDpos - 12.5 months (р=0.001). Medians OS were not achieved in both groups. 5-year OS were: group MRDneg - 83.8% and group MRDpos - 73.3%. 10-year OS were: group MRDneg - 64.4% and group MRDpos - 58.7%. When comparing OS in patients among all groups no significant differences were found, which is probably due to a small number of events (р>0.05).
Conclusion: Our data demonstrate that achievement MRDneg remissions determine duration of response on ongoing therapy and significant increase of PFS duration. Presently, MRD detection in patients with MCL is important part of complex assessment of effectiveness therapy and it need to be studied more.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal